
Five years from now, you'll probably wish you'd started investing with Stock Advisor
- New stock picks each month
- Detailed analysis of companies
- Model portfolios and advanced tools
- Live streaming during market hours
Featured Investing News


Billionaire Bill Ackman Has His Sights on Only 1 "Magnificent Seven" Stock, and It's Not Nvidia

These 3 Dow Stocks Are Set to Soar in 2024 and Beyond

This Small-Cap Stock Is Up 140% This Year and Here's Why It Can Go Even Higher

Peloton Stock Is Beaten Down Now, but It Could 10X
Trending News
- Tesla Just Shared Some Spectacular News for Nvidia Stock Investors
- With Shares Down Nearly 70%, I'm Piling Into this Ultra-High-Yield Dividend Stock
- Meet Eli Lilly's Secret Weapon in the Billion-Dollar Weight Loss Drug Market
- This 15%-Plus-Yielding Passive Income Stock Continues to Deliver Despite Persistent Challenges
- 1 Stock That Turned $2,400 Into $1 Million
- Tesla Sent a Clear Message to Wall Street on Tuesday
- History Says the Nasdaq Could Soar: 2 Top Growth Stocks to Buy Now and Hold for the Bull Market
- Forget Nvidia: Billionaires Are Selling It and Buying These 2 High-Octane Artificial Intelligence (AI) Growth Stocks Instead
- Forget Chipotle, Check Out This Up-and-Coming Fast Casual Restaurant Entrant
- 1 No-Brainer Vanguard Fund to Buy Right Now
- 3 High-Yielding Dividend Stocks That Can Help Bankroll Your Retirement Years
- 3 No-Brainer Stocks to Buy With $300 Right Now
- 2 No-Brainer Stocks to Buy Now With $200 and Hold Long Term
- Nasdaq Bull Market: 2 Growth Stocks to Buy Before They Soar 111% and 167%, According to Certain Wall Street Analysts
- I Was Incredibly Wrong About the Tesla Cybertruck
Popular Topics
About The Motley Fool
Our Purpose: To make the world smarter, happier, and richer.
Founded in 1993 by brothers Tom and David Gardner, The Motley Fool helps millions of people attain financial freedom through our website, podcasts, books, newspaper column, radio show, and premium investing services. We believe that investing is empowering, enriching, and fun. We look forward to joining you on your journey to financial independence. Learn More
The Motley Fool Investing Philosophy
Learn How We Invest-
#1 Buy 25+ Companies Over Time
-
#2 Hold Stocks for 5+ Years
-
#3 Add New Savings Regularly
-
#4 Hold Through Market Volatility
-
#5 Let Your Winners Run
-
#6 Target Long-Term Returns
Investing Solutions Designed To Make Money Over The Long Term
Become a member today

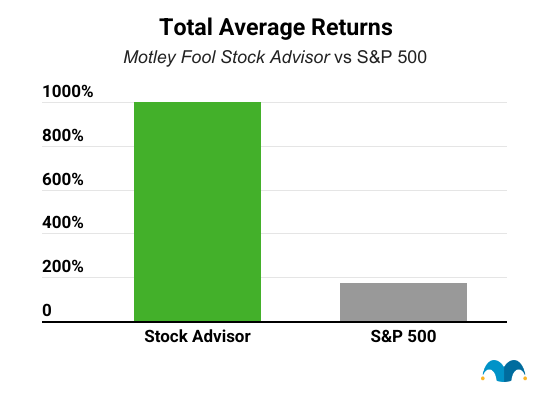
Stock Advisor
Our base-level-membership giving you the foundation of a Foolish portfolio
Help members earn a positive return and build the foundations of a portfolio backed by Motley Fool principles.
Individuals who are seeking easy-to-use guidance on investing in more familiar-named companies.
$5,000 +
- Monthly stock recommendations (usually large and mid-cap stocks)
- Portfolio allocation guidance via The Motley Fool's Allocator tool
- On-going coverage of prior recommendations
- Access to Motley Fool Live video stream

Epic Bundle
A bundled membership that combines our four foundational stock-investing services into one
Help members outperform the benchmark by gaining exposure to a wider variety of stocks and investments.
Individuals who are regularly adding new money to their brokerage accounts, interested in business, and want to spend more time learning the art of investing.
$25,000 +
- Includes access to Stock Advisor + Rule Breakers + Everlasting Stocks + Real Estate Winners
- Weekly stock recommendations (ranging from small to large-cap stocks)
- Portfolio allocation guidance via The Motley Fool's Allocator tool
- On-going coverage of prior recommendations from all included services
- Access to Motley Fool Live video stream